By Stuart Kurtz, D-ABFT-FT
In April, I spoke at the Midwest Association of Toxicology and Therapeutic Drug Monitoring (MATT) annual conference in Columbus, OH. The title of the talk was “Detection of Xylazine in Postmortem Specimens With Fentanyl, Morphine, Methamphetamine, and Cocaine From 2021-2022.” The conference was a great opportunity to talk shop with peers from the Midwest region and hear what they are doing. In this post, I will summarize what was presented at the MATT conference.
Xylazine was first synthesized as an antihypertensive by Bayer in 1962. During clinical trials, it was found to have additional central nervous system (CNS) depression effects. Despite being investigated for use as an antihypertensive agent, some patients would initially experience hypertension before the desired effect of a reduction of blood pressure. Some patients also experienced much more severe hypotension than intended. Due to these findings, it was rejected for human medical use and only approved for veterinary purposes.
A survey done by Texas Poison Control looked at the reported effects of xylazine toxicity. The major reported adverse effects were drowsiness and lethargy (47%), bradycardia (20%), hypotension (11%), hypertension (9%), and slurred speech (8%). Analgesic effects have been reported but the mechanism is not well understood, and the effect is minimal compared to its other adverse effects. There are two theories behind the mechanism. One immunoassay study found that xylazine could weakly displace opioids at binding sites. In this study, naloxone was not seen to reverse the effects. The other theory is that xylazine stimulates the release of endogenous opioids which could be reversed by naloxone. These are theories that have been reported but further study is needed.
Published case reports involving xylazine typically describe the presence of at least one other additional substance in combination with xylazine which may lead to an additive effect. When xylazine is the primary substance of toxicological interest detected in casework, there is a competing cause of death or an intentional overdose as determined by the scene investigation. The blood concentration range in these cases was 2,300-11,000 ng/mL. In cases of intentional overdose, the decedents worked in the veterinary field and had access to xylazine. The case involving a xylazine blood concentration equal to 2,300 ng/mL was ruled suicide by hanging after injection of xylazine. One attempted suicide case had a serum concentration of 4,600 ng/mL with the individual making a recovery with medical intervention. Two other fatal cases involving xylazine had blood concentrations of xylazine (200 ng/mL)/nordiazepam (2,500 ng/mL)/ and xylazine (300 ng/mL)/flualprazolam (1,100 ng/mL). In driving under the influence of drugs (DUID) casework, a range of 5.1-450 ng/mL of xylazine in blood was found. Full case histories were not available so it is unknown if any of those individuals died from effects of xylazine with other drugs that may have been present. A case of 570 ng/mL in blood was reported from a driver who passed out in their car but could be awakened.
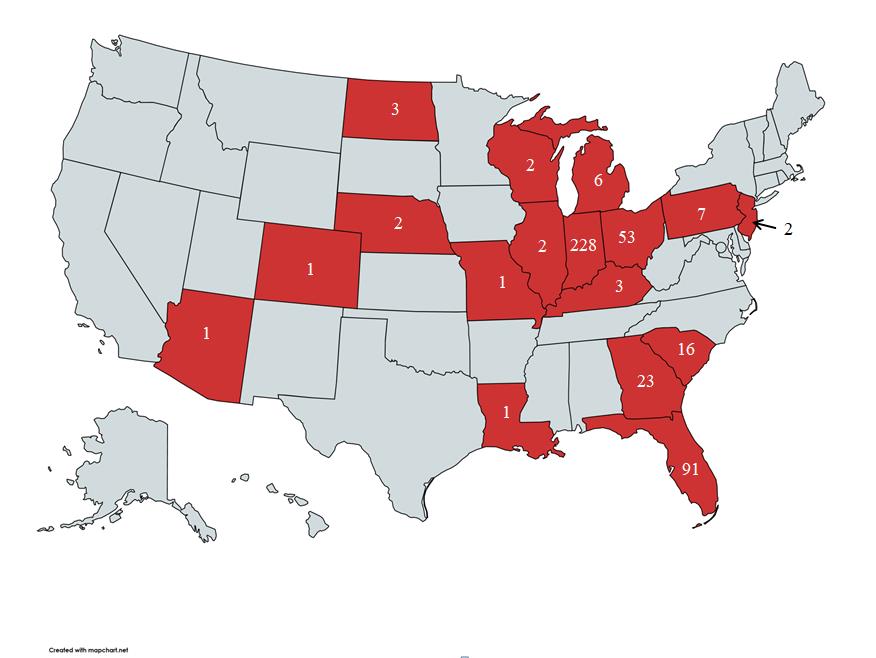
A heat map of xylazine detections based on data from Axis Forensic Toxicology’s lab.
For the years 2021-2022, we had 442 total detections of xylazine. For reference, we receive about 22,000-24,000 cases per year. The following drugs were commonly detected alongside xylazine: fentanyl (92%), benzoylecgonine (29%), methamphetamine (26%), morphine (12%). In 26% of the cases, the combination of xylazine, fentanyl, and methamphetamine was observed, while in 4% of the cases, the combination of xylazine, fentanyl, methamphetamine, and benzoylecgonine was detected.
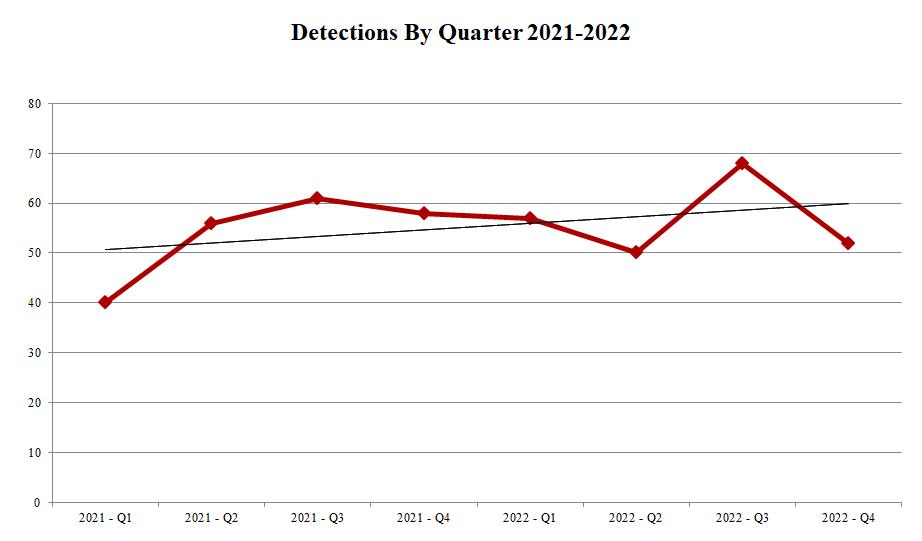
Xylazine detections by quarter have risen slightly since Q1 2021.
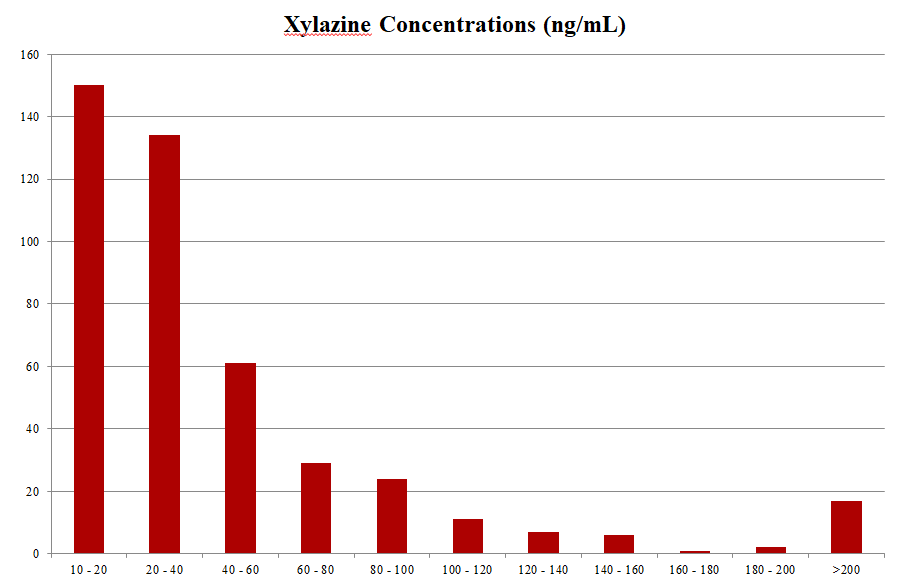
64% of xylazine detections fall in the concentration range of 10-40 ng/mL.
Because of the lack of data surrounding human clinical use of xylazine and the lack of reports of sole xylazine use, it is hard to determine what postmortem blood concentrations could be considered fatal. Xylazine is almost always found in combination with another drug due to its popular use as an adulterant. Its CNS depression effects can mimic other compounds such opioids and benzodiazepines and it is not scheduled as a controlled substance by the Drug Enforcement Administration (DEA) in the United States, so access is not very restricted. Because of its additive effects with other CNS depressants, it can still be relevant in postmortem toxicology, and it is included in our comprehensive panel of testing.
Wounds associated with xylazine use have been reported in Philadelphia, PA. We have not received any reports of wounds potentially associated with xylazine use. Also, in talking with other forensic toxicologists around the country, we have not heard from them any other reports of these wounds being present in their locations.
As always, please reach out to us if you have any questions about this post. We can be emailed at [email protected] or you can call us at 317-759-4869 option 3.
Sherri L Kacinko, Amanda L A Mohr, Barry K Logan, Edward J Barbieri, Xylazine: Pharmacology Review and Prevalence and Drug Combinations in Forensic Toxicology Casework, Journal of Analytical Toxicology, Volume 46, Issue 8, October 2022, Pages 911–917, https://doi.org/10.1093/jat/bkac049
Karla A. Moore, Mary G. Ripple, Saffia Sakinedzad, Barry Levine, David R. Fowler, Tissue Distribution of Xylazine in a Suicide by Hanging, Journal of Analytical Toxicology, Volume 27, Issue 2, March 2003, Pages 110–112, https://doi.org/10.1093/jat/27.2.110
Malayala SV, Papudesi BN, Bobb R, Wimbush A. Xylazine-Induced Skin Ulcers in a Person Who Injects Drugs in Philadelphia, Pennsylvania, USA. Cureus. 2022 Aug 19;14(8):e28160. doi: 10.7759/cureus.28160. PMID: 36148197; PMCID: PMC9482722.
Way Koon, Teoh & Muslim, Noor & Chang, Kah Haw & Abdullah, Ahmad Fahmi Lim. (2022). Abuse of Xylazine by Human and its Emerging Problems: A Review from Forensic Perspective. Malaysian Journal of Medicine and Health Sciences. 18. 190-201. 10.47836//mjmhs18.4.26.
